Regenerative Medicine
Tufts’ experts in biology and regenerative medicine are developing groundbreaking new frameworks for harnessing the mechanisms that allow multicellular bodies to self-assemble, repair, and improvise novel solutions to anatomical goals.
Harnessing the Power of Intelligent, Multicellular Bodies
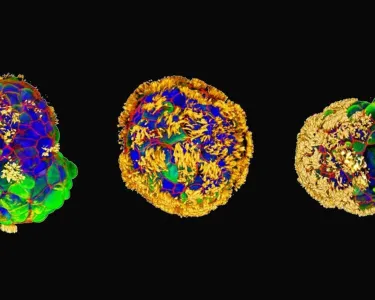
Working at the intersection of developmental biology, artificial life, bioengineering, synthetic morphology, and cognitive science, scientists at Tufts’ Levin Lab seek to understand diverse intelligences—including cells, tissues, organs, synthetic living constructs, robots, and software-based AIs—with the aim of revolutionizing medical care.
Led by Michael Levin, Vannevar Bush Professor of Biology in the School of Arts and Sciences, researchers at Levin’s lab and at the Allen Discovery Center take an interdisciplinary approach to reading, interpreting, and writing the morphogenetic code. That code, an instructive layer of biophysical computations, lies between the genomically specified protein hardware of cells and the complex anatomy; it orchestrates and enables cells to communicate to create and repair the structure and function of bodies.
Applying that knowledge, Tufts’ experts have regrown a frog’s lost leg, bringing millions of patients who have lost limbs one step closer to the possibility of regaining function through natural regeneration. They have also created the next generation of living robots, tiny “Xenobots” that self-assemble a body from single cells, move without muscle cells, demonstrate the capability of recordable memory—and even self-replicate.
Ongoing work at the Tufts Center for Regenerative and Developmental Biology promises additional advances in the field, with researchers at the center using a combination of wearable bioreactors and small molecule drug regimes to trigger rodent limb regeneration and demonstrating a new bioelectric method to regulate innervation from organ transplants.
Selected Research
Areas of Exploration
-
Understanding the role of the nervous system in regeneration
Tufts scientists developed a computational model of planarian (flatworm) regeneration that explains how fragments of planaria determine which end should form a tail and which should form a head. The development begins to answer an important question in regeneration research: What are the signals that determine the rebuilding of specific anatomical structures?
-
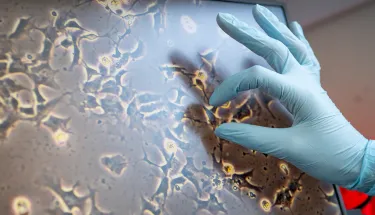
Reconstructing Sensory Nerves and Tissue Structures
A team of researchers at Tufts University School of Medicine developed a method to grow and maintain olfactory stem cells in culture, which can then be used to restore tissue in the nose. The discovery raises hope that future therapies could be developed to restore the sense of smell in individuals in whom it has been damaged by injury or degeneration.
-
Speeding Up Wound Healing
Researchers at Tufts are using small electronic devices that attach to wounds and applying lessons from machine learning and regenerative medicine, with the aim of achieving precise control over the physiological processes involved in wound healing.
-
Preventing or Repairing Birth Defects
In work that could provide a road map for the exploration of therapeutic drugs to help repair birth defects, Tufts biologists have discovered that the brains of developing frog embryos damaged by nicotine exposure can be repaired by treatment with drugs called ionoceuticals. These drugs drive the recovery of bioelectric patterns in the embryo, followed by the repair of normal anatomy, gene expression, and brain function in the growing tadpole.